The Psychosis Prodrome.
Psychotic disorders are devastating for individuals and their families as they involve the onset of symptoms and significant impairment during adolescence and young adulthood- two critical developmental periods when youth are only just starting to make a transition into independence. These disorders are highly prevalent (impacting between 1-2% of the population), and once diagnosed, involve a chronic course and challenging prognosis. However, an emerging research field suggests that we can now effectively identify those who are at imminently high-risk for psychosis, several years before onset (Figure 1).
Figure 1. Model of Psychosis Onset in Schizophrenia. Symptom severity, as indicated on the y-axis, is lower in the earlier than later stages of the disease, as indicated by the x-axis. Source: Fusar-Poli P, et al., JAMA Psychiatry. 2013;70(1):107-120.
High-risk syndromes are defined, in part, by attenuated positive symptoms (e.g., experiencing unusual thoughts, seeing brief shadows, hearing strange sounds). Individuals with these syndromes also show persistent difficulties with motor, perceptual, cognitive and emotive functioning. Cumulative changes during the high-risk (or prodromal period) result in significant impacts in social, academic and occupational functioning. Those who meet the criteria for a high-risk syndrome have a chance of developing schizophrenia or an affective disorder with psychotic features within a two-year period. This serves as a foundation for a line of research that suggests that if we can identify high-risk adolescents and young adults and provide early intervention, the course of illness will be improved or perhaps prevented entirely.
How Can We Conceptualize the Prodrome?
In a neural diathesis-stress conceptualization of psychosis, individuals with a biological susceptibility (i.e., from inherited genes, mutations, and early prenatal teratogen/insult) often exhibit subtle signs of impairment from infancy and then carry these signs forward throughout childhood (e.g., delayed achievement of milestones such as walking/talking/toilet training; motor abnormalities; poor social skills and affective responsivity; cognitive deficits).
Figure 2. Mittal & Walker, 2019
Much later, these vulnerabilities interact with the substantial environmental stressors and dramatic neural and endocrine maturational factors that occur during adolescence and early young adulthood. During this time normative age-related increases in sex hormones synergistically affect neurotransmitters and modulate gene expression. Further marked neural reorganization affects both connectivity and intercommunication between key brain structures and networks. It is also important to consider that the adolescent and young-adult time periods are characterized by a significant number of major life-stage decisions, as well as increases in everyday stressors and responsibilities. Each of these social requirements involves making adult decisions without the benefit of a fully developed adult brain (e.g., limiting impulsive thinking and promoting efficient thinking). This can place an additional burden on a progressively compromised system (indeed, one common experience is feeling more "thrown-off" by everyday stressors). Finally, individuals in these stages are often exposed to additional environmental stressors including substance abuse. Together, the early vulnerability interacts with adolescent and young-adult developmental factors as well as social and environmental stressors, contributing to emerging subtle attenuated psychotic symptoms. Some common symptoms include: finding a greater degree of meaning in everyday coincidences (aberrant salience), seeing shadows out of the corner of one’s eye, mild grandiosity, feeling vaguely suspicious of friends and family and experiencing increasing difficulty in getting one’s point across. In addition to these symptoms, adolescents and young adults in the prodrome often report negative symptoms (e.g., feeling low motivation, not enjoying things that were previously held to be pleasurable, feeling emotionally disconnected from the self or others), as well as difficulties with cognition (this can present as difficulty concentrating and increasing difficulty in school or at work) and emotional processing (this can present as exhibiting increasing difficulty with processing and interacting with social situations). In turn, these emerging symptoms lead to increased stress, which may tax progressively compromised neural and hormonal systems. Indeed, because stressors influence hormones, and because of the important role that hormones (including stress hormones) play in regulating genes responsible for guiding brain development, the noted difficulties and environmental stressors can impair neural development, and consequently, contribute to further vulnerability. This may drive a cascade which eventually drives the onset of formal psychosis.
Why Does Development Matter?
Vargas & Mittal, Annual Rev Dev Psychol, 2022. Expanding the diathesis-stress model (see Figure 3a) to consider early development as well as dynamic and multifaceted environments, stressors, and systemic factors. Abbreviations: ACTH, adrenocorticotropic hormone; DHEA, dehydroepiandrosterone; DHEA-S, dehydroepiandrosterone sulfate; HPA, hypothalamus-pituitary-adrenal; HPG, hypothalamic-pituitary-gonadal.
Figure 3b. Normal cortical development involves proliferation, migration, arborization, and myelination, with the first two processes occurring mostly during prenatal life and the latter two continuing through the first two post-natal decades. The combined effects of pruning of the neuronal arbor and myelin deposition are thought to account for the progressive reduction of grey-matter volume observed with longitudinal neuroimaging. Beneath this observed overall reduction, local changes are far more complex. . b. The trajectory in children developing schizophrenia could include the reduced elaboration of inhibitory pathways and excessive pruning of excitatory pathways leading to altered excitatory-inhibitory balance in the prefrontal cortex. Reduced myelination would alter connectivity. Detection of prodromal neurodevelopmental changes could permit early intervention with potential prevention or preemption of psychosis. Source: Insel, 2010 (appearing in Nature)
Although serious mental illness can occur during a number of developmental periods, a majority of cases first develop at the end of adolescence and the beginning of young-adulthood. As a result, it has become increasingly clear that developmental factors play an important pathogenic role. As seen in Figure 3a,b, significant brain reorganization during adolescence and young adulthood overlap with the emergence of symptoms. At the same time, the hormone system is highly active, regulating puberty by governing genes that modulate synaptic pruning and white-matter development. Both developmental systems are highly sensitive to environmental and social factors as well. Because of the emphasis on development in understanding factors in the high-risk period, we also focus each of our research questions within this context. With this in mind, the lab is dedicated to longitudinal research, and we employ a range of experimental paradigms and methodologies to assess the same individuals at different developmental time points. We are particularly interested in how factors contribute to early vulnerability, and then, how environmental factors occurring during adolescence and young adulthood, as well as brain and hormone development in this period, unmask this vulnerability, leading to emerging symptoms and other characteristics that impair quality of life and contribute to disability in these individuals.
What are the Priorities for Research in this Area?
The available research has consistently shown that roughly 10-35% of adolescents and young adults exhibiting a prodromal or high-risk syndrome (i.e., based on the course, frequency, and severity of a combination of the symptoms and characteristics noted above) will convert to a psychotic disorder within a two-year period.
A growing body of evidence also suggests that early intervention may be helpful for those at risk for psychopathology. Specifically, forming relationships with treatment providers prior to serious illness, adopting strategies before severe and acute symptoms can interfere with the acquisition and assimilation of psychotherapy skills (e.g., stress management), engaging family members in both reducing the stressful environment and helping to monitor the subtle changing symptoms, and/or beginning treatment can ameliorate course of illness and may help to delay or even prevent onset of a psychotic disorder.
Unfortunately, although we know that approximately 1/3rd of high-risk individuals will convert to a psychotic disorder in a short period of time, we are not certain of whom among the at-risk group is most likely to fall into this category. As blanket treatment for all high-risk individuals is not a feasible method for intervention (due to costs of psycho-social and pharmacological interventions as well as ethical concerns relating to medication side-effects), identifying those individuals at highest risk for this conversion is an urgent and important research priority. Further, developing new effective targeted treatments (capable of treating symptoms and characteristics that are impairing, but have yet benefited from effective interventions) is critical. Our belief is that we can use data from longitudinal and experimental investigations to inform early identification and intervention.
What is ADAPT doing about it?
Research Areas
This period of transition during adolescence and young adulthood (i.e., the prodromal or high-risk period), immediately before the formal onset of psychosis, holds the unique potential to both inform etiological conceptualizations of psychotic disorders, and serve as a viable point for early intervention and/or prevention.
To date, the ADAPT lab has specialized in several distinct, but mechanistically related susceptibility markers, behaviors, and symptoms that reflect 1) disordered communication between the subcortical structures that govern basic human function and the frontal regions that underlie higher-order functions, 2) abnormalities in medial temporal brain structures and function and 3) dysfunction in emotional systems and dynamic social interaction. We have focused on these phenomena because they appear to interact with developmental and genetic factors, share related neurological underpinnings that also characterize psychosis, directly contribute to poor quality of life (or, if not, can directly inform treatment development efforts), and are quantifiable, potentially enabling a system of early identification and intervention.
Details from each of these studies can be found on the lab publication page
Basal Ganglia and Cerebellar Circuits
Psychotic disorders are characterized by distinct domains of symptoms as well as emotional, nonverbal, and cognitive deficits drawing upon a host of disparate mechanisms and structures. Our first line of research tests the idea that the basal-ganglia circuits, which are responsible for dynamic communication between the subcortical structures that govern basic functions and the frontal regions that underlie higher-order functions (e.g., cognition, perception, motivation/reward, emotion), are a good target for improving our understanding of why such a wide variety of functions are affected in psychosis (Figure 5; from Obeso et al.). Current thought holds that markers of dysfunction in one structure or circuit will also be indicative of dysfunction in other loops (as the circuits are governed by the same neurotransmitter systems). Within this context we have been particularly focused on domains of motor behavior (e.g., gesture) and types of movement dysfunction (dyskinesia, soft signs, dyspraxia), as these characteristics reflect basal-ganglia circuit dysfunction as well as dysfunctional integration between the basal ganglia circuits and other relevant domains.
Figure 5. Basal ganglia loops are relevant for significantly more than motor behavior. Loops are integral for governing executive function, motivation/reward, and personality (Obeso et al., 2014, Lancet).
Basal ganglia, cerebellar, and cortical loops govern motor behaviors, and dysfunction across these circuits is implicated in the pathophysiology of psychosis.
Figure 6. Participants in the ultra high-risk group show increased sway area when compared to controls. Our lab uses a highly sensitive multiaxial postural control device.
Further, as these circuits are influenced by inflammation, there is significant promise for understanding this work in broader conceptual frameworks. In addition, approaches such as transcranial direct current stimulation (tDCS) hold significant promise for elucidating specific aspects of these circuits and employing novel interventions. In following this line of inquiry, we have also focused on how basal ganglia circuit pathology affects characteristic domains of psychosis including emotion, perception, cognition, and reward. In addition, we have expanded the study in this area to the cerebellar circuits- another critical system that is affected in schizophrenia and believed to govern coordination and balance as well as synchronize cognitive functions (see Figures 6-7). Our preliminary work in this area suggests that the cerebellar system may account for a unique category of symptoms and cognitive deficits. Our current efforts focus on integrating the two systems to provide a better understanding of unique and overlapping contributions to symptom domains and areas of cognitive function; these efforts hold the potential for supplementing traditional observer symptom-based classification system with a biologically based approach (more akin to diagnosis in medicine).
There is a significant translational component to this research program that applies specifically to early identification. As noted, approximately 10-33% of high-risk individuals go on to develop psychosis, but because we don’t know which of the initial cases (who exhibit similar clinical presentations) will be in this group, blanket intervention is not feasible (due to costs and side effects associated with many of the currently available treatments). Our work with biomarker development has significantly helped to improve efforts to identify which individuals in this initial group are most likely to develop psychosis.
Figure 7. We adapted a force variability task utilizing polymer rods and air pressure for use inside the scanner (with the help of Randy O'Reilly and his team). This fMRI task has helped us to understand frontal-striatal contributions to deficits in motor control.
We have also been working with researchers to develop tools that can be used to disseminate these findings to clinical settings and be applied to improve treatment decisions. For example, we are working with a team developing a program for analyzing pen dysfluencies in handwriting (possible to be assessed on any tablet computer), and our preliminary results suggest by focusing on specific markers, we can accurately detect the same movement abnormalities that previously would have required a highly specialized neurological training background. With regard to the cerebellar circuits, we have recently reported findings that suggest that deficits determined by a brief neurological battery can significantly predict abnormalities in cerebellar-thalamic white matter tracts that are tied to progressively worse symptoms. As a result, clinicians who do not have access to neuroimaging facilities may also be able to identify patients in the greatest need of intervention.
Additionally, we are focusing on vocal analysis- the voice (which involves complex coordination between a variety of muscle groups) is a sensitive indicator of motor function, and many important clues can be derived by focusing on abnormal features such as fluctuation. The lab is collaborating with linguists as well as computational scientists to link subtle emerging vocal anomalies to cerebellar circuits and to the progression of psychosis.
We are also launching a new treatment development study, evaluating if cerebellar stimulation is effective in improving verbal working memory deficits in early psychosis. In this context, our lab will be one of the first to utilize tDCS in conjunction with fMRI (participants will receive sham or active stimulation immediately proceeding the scan session), and this approach will provide a significantly improved understanding of how cerebellar-thalamic circuit dysfunction contributes to verbal working memory deficits in psychosis, and further, how brain stimulation modulates activity in this vital circuit. This will help to lay the foundation for innovative new treatments targeting areas that significantly contribute to disability, such as cognition.
Finally, the lab is collaborating with an international group of scientists and helping to lead the effort to understand motor pathology as it occurs across different forms of serious mental illness including affective disorders. Recently PI Mittal was working with the NIH RDoC workforce to help develop a system for understanding different aspects of motor pathology (added officially now), with hopes that a clear framework would drive translational (clinically relevant) research. For example, if patients with recovered depression begin to show slowing or less movement, or in contrast, increased agitation (as assessed with a smartphone app), a clinician or provider might then know to adjust treatment parameters. Our team recently received an award to examine motor dysfunction in this way and to link it to changing brain circuitry, across stages of major depressive disorder.
Hippocampal Function, Stress, and Exercise Interventions
Figure 8. Exercise Model of Psychosis: Mittal
The hippocampal system, responsible for moderating biological stress reactivity as well as integral cognitive functions, is highly implicated in psychosis as it may serve as an interaction point between the environment and underlying biological susceptibility. Our second line of research focuses on hippocampal development (longitudinal changes in shape, structure/connective tracts, and function), interactions with psychosocial stress and related hormones such as cortisol (using paradigms involving life-events and expressed emotion/family environment, and Social Stress Tests) and causal factors underlying system vulnerability (e.g., obstetric complications, inflammation). For example, in one longitudinal investigation, we found that hippocampal shape anomalies predict a poorer course of illness for those at psychosis risk. Recently, we have also observed that the family environment influences resting levels of stress hormones, and that self-concept may moderate this relationship.
There are several translational components to this work that we are particularly enthusiastic about. It is important to consider that while several of the available treatments for individuals at high-risk for psychosis have been found to show some promise in terms of improving prognosis and cognitive function, including cognitive training (which acts upon hippocampal mediated synaptic plasticity). To this end, we have been particularly interested in translating the findings from our longitudinal naturalistic studies into a viable treatment for high-risk youth. Most recently, we have begun to develop a related line of research examining how hippocampal development is affected by physical activity in at-risk youth. Because the hippocampus is a critical structure for de-escalating the stress response, has been found to develop abnormally in high-risk adolescents, and is believed to contribute to cognitive dysfunction, this structure is a key treatment target (Figure 11). If we can harness aerobic exercise, an activity that is widely available, inexpensive, and accompanies few side-effects, this could have a significant public health impact.
Emerging literature suggests that regular aerobic activity can stimulate hippocampal neurogenesis and we have begun to investigate the potential for an exercise intervention for high-risk youth. In an initial study, we found that high-risk youth engaged in significantly more sedentary and less aerobic activity than controls (assessed with actigraphy over a 5-day period) and that inactivity was associated with smaller medial temporal structures in this group. Following this investigation, we collaborated with Angela Bryan (Co-PI) to propose a related intervention and the study was funded through an innovative translational award that combines a phase 1 stage (to test the underlying mechanism and fine-tune the treatment parameters) and a phase 2 randomized controlled trial (RCT). In this ongoing study, we are working to determine if prescribed exercise (monitored exercise for 3 times a week for 12 weeks) will lead to better fitness (V02 Max), hippocampal cell growth, improved episodic memory, and reduced symptoms in this critical population.
We are also preparing to examine if brain-derived neurotrophic factor (BDNF) RNA expression changes as a function of aerobic exercise and if it, in turn, mediates the beneficial relationships between exercise and the brain. As exercise may indeed influence factors such as synaptic plasticity, this work has significant potential for future trials conducted in conjunction with treatments involving cognitive training (Figure 8).
Emotion and Social Interaction
As youth at risk for serious mental illness progress in adolescence, insidious deficits in emotional perception, interpretation, and expression begin to interfere with social interaction. This can stunt growth in a time when youth are supposed to be enjoying experiences and learning lessons that help to set the stage for a lifetime. These emotional and social difficulties can also push away support networks and foster isolation and stigma, eventually contributing to the course of illness. It is a very important and nuanced area of development. For example, some core emotional areas appear to be intact in early psychosis (e.g., experience), but others are affected (the extent to which past experiences motivate future behavior); one possibility is that influence from other systems, including deficits in cognition (impacting reward learning), stress sensitivity, or motor impairment (e.g., disrupting efficient or coherent performance of non-verbal communication) may play a role. Our approach, focusing on linking together information from other systems, is ideal for addressing the complexity of these issues. This stems from a heartfelt desire to translate findings from basic research into meaningful interventions that are practical and can impact public policy. To this end, we have been working to develop a research program examining social processing across domains, and using multiple layers of assessment (e.g., ranging from self-report to behavior, to complex behavioral interaction, to brain activity).
Figure 10. Familiarity may not lead to a habituated neural response over time in youth at-risk for psychosis and this may contribute to broader functional impairments. (Osborne..Mittal, 2021, JoPaCS)
While working in this area, the lab has become discouraged by the lack of assessment tools that are informed by empirical work. For example, currently available scales conflate behaviors (e.g., not going to parties) with internal experience (this must mean they do not want to go to parties), where in reality, the two are quite separable (e.g., social anxiety might lead to a behavior such as avoiding parties, but the existing scales would mark this as disinterest). We are collaborating with Emory and the University of Georgia (Gregory Strauss) to develop a promising new measure (a preliminary version of the measure can be found here). The project also recently received funding from NIH and we plan to develop and thoroughly validate the scale as well.
Figure 9. Dyadic interaction study rationale
The ADAPT team has also been interested in elucidating the basis of social interaction deficits in high-risk youth. The lab has published a number of related studies on social cognition/theory of mind and also looked at non-verbal behaviors such as gestures that may impact communicative ability. We also have examined factors contributing to feelings of peer group isolation. The lab is currently is running a large gesture assessment battery incorporating a data glove and VR technology to look at these deficits across interpretation as well as perception and action. Most notably, together with Claudia Haase (SEPI), we plan to examine dyadic interaction between adolescents at high-risk and their parents, designed to determine if emotional dysregulation and impacted empathy might predict the course of illness in the adolescents, and immediate and long-term health outcomes in the care-takers (Figure 9).
Finally, ADAPT has been putting a lot of attention into approaching emotional dysfunction from a brain-based perspective. For example, we recently published a report examining the resting state correlates (using salience network seeds) of deficits in facial emotion recognition and are currently running a related eye-tracking paradigm. We have also recently completed a novel social reward fMRI study and begun recruitment for an fMRI study adapting a monetary incentive delay (MID) task for use in high-risk youth. In addition, in an ongoing study, ADAPT is examining the neural basis of facial emotion deficits in youth at risk for psychosis using a novel event-related potential paradigm (Figure 10). It is currently unclear if misattribution (seeing angry/fearful instead of happy) or trouble with becoming accustomed to familiar faces contributes to social functioning issues that impact the quality of life in many youths at risk for psychosis. This information is vital for developing new treatments as the targets would differ significantly based on early and late deficits in neural processing.
Methods
The ADAPT lab specializes in focusing on the brain, endocrine, and motor changes during adolescence and young adulthood with the goals of:
Figure 11a. Lab members Tina Gupta and Katherine Damme perform pre-processing and quality checks utilizing the lab’s graphics workstation.
Understanding the role of development in emerging psychopathology
Identifying biosignatures
Informing innovative treatments
Our guiding mission is to translate knowledge from basic science approaches to practical and widely disseminable biomarkers and targeted interventions. To accomplish these goals we utilize naturalistic (longitudinal) and experimental behavioral paradigms.
11b Kate's project, currently under review with a great journal, examines cortical surface morphometry from several different angles.
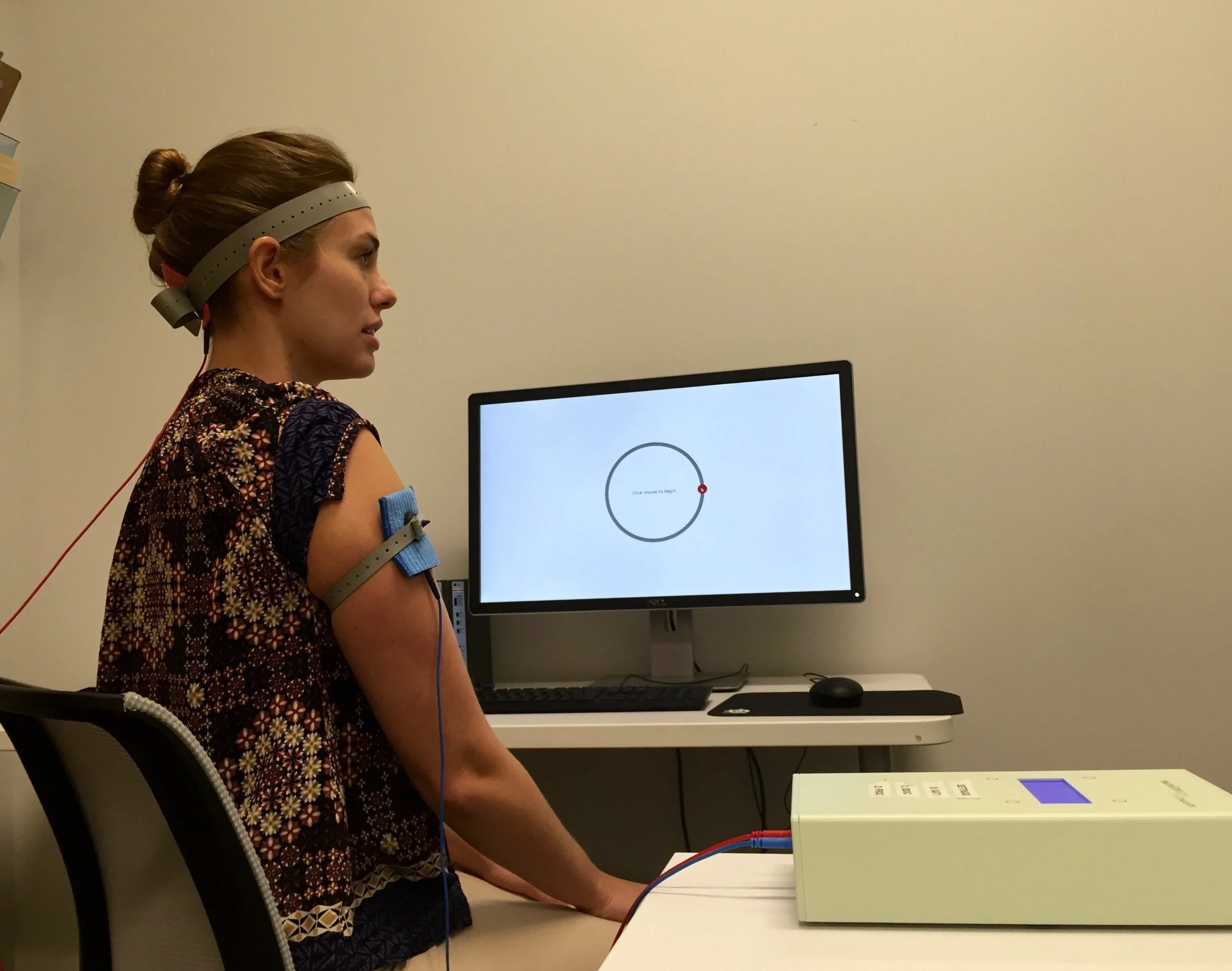
Figure 12. Depicts Cerebellar tDCS that is applied in an ongoing study designed to improve implicit learning rates.
The ADAPT lab employs innovative methodologies for examining our guiding research questions (involving frontal subcortical circuits, hippocampal function, neural/endocrine development, and emotion/social dysregulation) as well as mediating factors (e.g., substance use and inflammation). Collectively, we employ advanced multi-modal brain imaging (Figure 11a,b), instrumental and VR assessments of movement and cognitive behavior, automated nonverbal behavior and emotive evaluation, hormone analysis (blood, saliva, and hair analysis), transcranial direct current stimulation (tDCS) (see Figure 12), auditory analysis, experienced sampling/actigraphy, stress sensitivity, aerobic fitness assessment (V02 Max), computerized linguistic and semantic analysis, eye tracking (employing paradigms at both 150 and 1000 Hz paradigms), electroencephalography (EEG), event-related potentials (ERPs), electromyography (EMG), dyadic interaction, and inflammatory marker, DNA and RNA analysis. Students interested in working with ADAPT will have the option to work with any of our primary or collaborator-guided methodologies. Participants who prefer to not participate in a particular component are still largely welcome to participate in those areas that they do feel comfortable with.
Other Interests
In addition to the primary research lines noted above, we are also interested in several other side studies involving graduate student projects that may eventually develop into more formalized programs and larger grant applications. These fall under the umbrella of the lab mission (promoting etiological understanding and identifying vulnerability makers of risk for developing psychotic disorders), but also reflect substantial student-guided interests as well (that they can carry on to their own labs in the future: e.g., sleep, social reward, Internet use, working memory).
The ADAPT lab is also dedicated to improving classification and assessment. To this end, we have authored several critical commentaries, reviews, and communications pertaining to the classification of movement abnormalities in psychiatric illness. In addition, the lab works to write peer-reviewed commentaries of assessment issues that are informed by experiences with at-risk youth.
We are also passionate about mental health advocacy and public policy. We are incredibly proud of a collaboration with Elyn Saks (Professor of Law at USC and prestigious mental health advocate) to evaluate ethical and legal dilemmas inherent in disclosing an attenuated psychosis syndrome diagnosis to patients and families and most recently, are editing a special issue of the Journal of Ethics in Mental Health on the topic of ethical considerations surrounding prodromal research and treatment.
Development of a Psychosis Risk Screeners for our Broader Communities
ADAPT has become very interested in improving our ability to detect psychosis risk in the general population. Currently, we focus entirely on help-seeking individuals, but by the time they come into the clinic, it is most often quite late. We would be able to help people more effectively, and understand the causes of psychosis better if we could get them identified as early as possible. In collaboration with colleagues at Temple and the University of Maryland, we recently received significant funding to evaluate risk markers in 12,000 adolescents across Chicago, Philadelphia, and Baltimore. In the first study of its kind, we will focus on using item response theory to develop a short screener that will let teens and practitioners in a variety of primary care or educational settings know that more in-depth screening might be required. In addition to being able to develop a helpful instrument, this opportunity will allow us to develop a cohort that we will propose a study, enriching collection and broadening our questions and approaches, for the next two decades. In addition, we are working with Temple, Yale, UMBC, UC Irvine, UGA, and Emory to develop a computerized battery of tests that may help to tie into mechanisms driving the onset of illness. This could potentially allow for a screener sensitive to emerging illness, and improve prediction as well. Finally, we are a proud member of PRONET, a global network of more than 25 specialized sites, working together with a common battery of tests, to understand and build a infrastructure for developing novel treatments for the psychosis prodromal syndrome.
Future Directions
In addition to the above research, ADAPT has many interesting ongoing projects that cover a variety of different methods and research interests within the field of psychosis risk. If you’re interested in learning more about our active studies, please click here to see a list of our ongoing studies with links to their descriptions!